
Health insurance rates are going up, and if you’re shopping on the individual marketplace, you’ve probably noticed. Utah’s market rates have already increased, and with premium tax credits set to expire December 31 we’re looking at additional increases for next year––which is why these aren’t your typical year-over-year adjustments.
At Ark Insurance, it’s our job to stay on top of these changes, and based on what we know so far there are a few strategies that might help you save some money.
The Big News: HSA Rules Just Changed (In a Good Way)
Starting January 2026, any bronze or catastrophic plan you buy through the marketplace automatically qualifies as HSA-compatible. This could be a real tax-saving opportunity.
Until now, a lot of bronze plans didn’t qualify for an HSA because of either high deductibles or copays. But with this new change, you can now pair an HSA with any bronze plan purchased through the healthcare.gov marketplace.
For 2026, you can contribute up to $4,400 for individual or $8,750 for family HSA coverage, all tax-deductible. If you’re over 55, you can tack on another $1,000. That money is tax-free for medical expenses, and rolls over every year.
Shifting Down the Metal Tiers
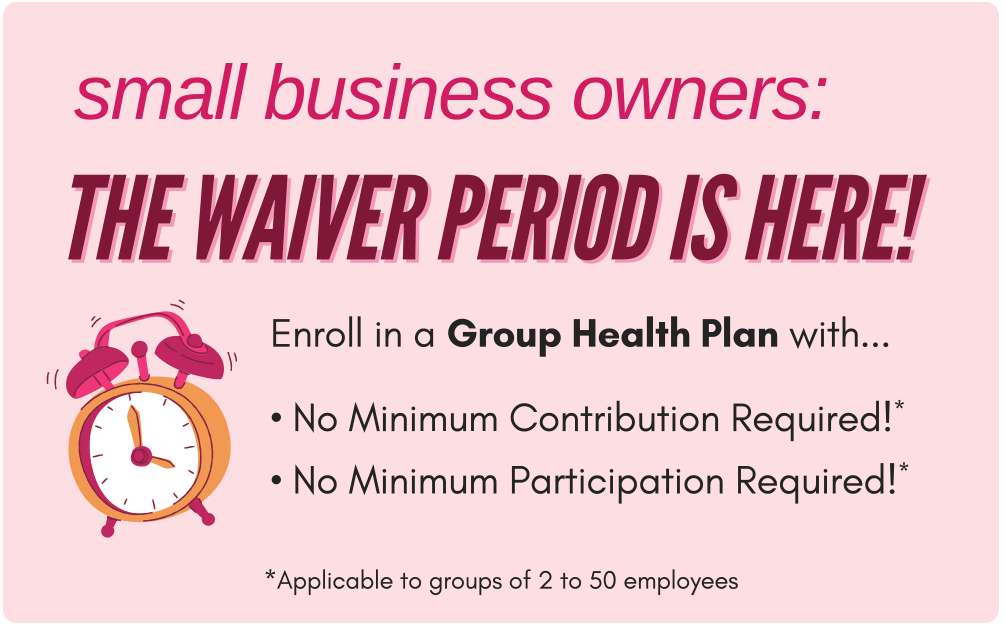
 What happens when premiums go up? Customers drop their plans down a tier. Gold to silver, silver to bronze. We’re seeing a lot of people make these shifts, and it is one way to help reduce your monthly payment.
What happens when premiums go up? Customers drop their plans down a tier. Gold to silver, silver to bronze. We’re seeing a lot of people make these shifts, and it is one way to help reduce your monthly payment.
If you’re thinking of shifting tiers, keep in mind there is a trade-off. Expect higher deductibles and more out-of-pocket costs if you actually need care. This is where the HSA rules can be useful. If you’re moving to a bronze plan, you can set up an HSA account for medical expenses and save some tax dollars. It doesn’t eliminate the risk, but it does give you a better way to manage it.
This strategy works best if you’re relatively healthy and can handle higher upfront costs in exchange for lower monthly premiums. It’s not right for everyone, and we recommend a consultation to better understand how a lower tier would affect you.
Pay Close Attention to Networks
As rates increase, carriers are tightening their networks to control costs. Whether or not this will affect you will depend on where you live and your health insurance plan. So if you’re thinking about a cheaper plan, just know that it might mean fewer doctors and hospitals you can actually use.
Before you buy a plan at the lowest price, make sure to check:
- Your current doctors and specialists
- Your preferred hospital
- Your pharmacy
- Any medications you’re taking
What About Catastrophic Plans?
 You might have heard the news that catastrophic plans are getting expanded. They used to only be available if you were under 30 or qualified for a hardship exemption. Now, they’re open to people making over 400 percent of the federal poverty level, and they also qualify for HSAs.
You might have heard the news that catastrophic plans are getting expanded. They used to only be available if you were under 30 or qualified for a hardship exemption. Now, they’re open to people making over 400 percent of the federal poverty level, and they also qualify for HSAs.
However, there is one problem. Most carriers haven’t filed these types of plans, and Utah does not have access to any catastrophic plans for 2026. It’s worth knowing about in case things change down the road, but unfortunately it isn’t a strategy you can use right now.
Why This Year Feels Different
If you feel like the health insurance landscape this year is a bit more confusing than normal, that’s because it is. The government shutdown and pending decision about expanding tax credits have created a level of uncertainty that is unusual, making it even more difficult to navigate important decisions about your healthcare. Staying current on rate filings, network changes, legislative updates, and carrier announcements is what we do here at Ark Insurance. When something changes mid-year or new regulations come through, we’re already tracking how it affects our clients.
Get in touch with us to figure out which strategies make the most sense for your situation. We’re here to help you sort through the noise and find coverage that works.
 Navigating the complex world of health insurance can be daunting. The Ark Insurance Solutions team has the skill and experience to guide you. We’ll help you compare health plans to make the best decision based on your unique circumstances and budget. Give us a call at 801-901-7800 or click here to schedule an appointment with us.
Navigating the complex world of health insurance can be daunting. The Ark Insurance Solutions team has the skill and experience to guide you. We’ll help you compare health plans to make the best decision based on your unique circumstances and budget. Give us a call at 801-901-7800 or click here to schedule an appointment with us.







 Already, Utah’s individual market rates have jumped considerably. Stack that on top of the upcoming tax credit expiration, and people buying individual marketplace plans are looking at increases as high as 438% in what they’ll actually pay.
Already, Utah’s individual market rates have jumped considerably. Stack that on top of the upcoming tax credit expiration, and people buying individual marketplace plans are looking at increases as high as 438% in what they’ll actually pay.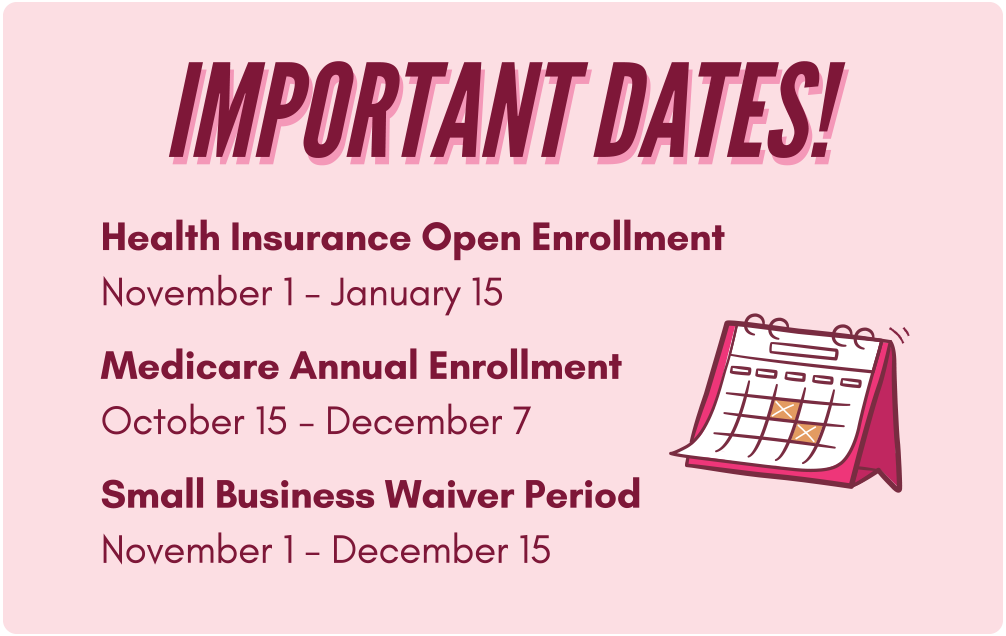 How We Can Help
How We Can Help

 What happens when premiums go up? Customers drop their plans down a tier. Gold to silver, silver to bronze. We’re seeing a lot of people make these shifts, and it is one way to help reduce your monthly payment.
What happens when premiums go up? Customers drop their plans down a tier. Gold to silver, silver to bronze. We’re seeing a lot of people make these shifts, and it is one way to help reduce your monthly payment. You might have heard the news that catastrophic plans are getting expanded. They used to only be available if you were under 30 or qualified for a hardship exemption. Now, they’re open to people making over 400 percent of the federal poverty level, and they also qualify for HSAs.
You might have heard the news that catastrophic plans are getting expanded. They used to only be available if you were under 30 or qualified for a hardship exemption. Now, they’re open to people making over 400 percent of the federal poverty level, and they also qualify for HSAs.

 The timeline is tight. Congressional recess begins December 19th, which doesn’t leave much time for negotiation between now and then.
The timeline is tight. Congressional recess begins December 19th, which doesn’t leave much time for negotiation between now and then.
